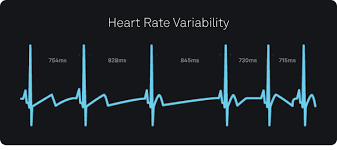
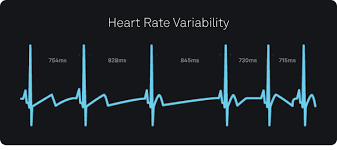
Heart Rate Variability is a key biomarker of autonomic nervous system health, reflecting the balance between the sympathetic and parasympathetic systems. Many people wonder whether beta blockers help or harm HRV.
The answer depends on context. Beta blockers can both increase and decrease HRV.
How Beta Blockers Affect HRV
Beta blockers work by blocking adrenaline's effects on the heart, slowing heart rate and reducing blood pressure. Their impact on HRV varies:
Short-Term Effects: Beta Blockers Often Lower HRV
In healthy individuals, beta blockers can reduce HRV by dampening sympathetic nervous system activity. Studies show decreases in time-domain HRV measures like SDNN and RMSSD when taking beta blockers.
Long-Term Effects: May Improve HRV in Certain Conditions
In heart disease patients, beta blockers can increase HRV by preventing harmful sympathetic overdrive. For hypertension, some beta blockers like nebivolol may improve autonomic balance over time.
Depends on the Type of Beta Blocker
Non-selective beta blockers like propranolol have the strongest HRV reduction. Cardioselective beta blockers like metoprolol have moderate HRV reduction. Vasodilating beta blockers like nebivolol may have neutral or slightly positive effects.
Should You Take Beta Blockers If You Track HRV
For healthy individuals using beta blockers for anxiety or performance, they might lower HRV temporarily. For those with heart disease, beta blockers may improve HRV. Those using wearables should discuss HRV changes with their doctor.
Final Verdict: Do Beta Blockers Help HRV
Beta blockers may help HRV in heart disease by reducing harmful sympathetic overactivation. They may lower HRV in healthy individuals. The effect depends on the type, with newer vasodilating beta blockers potentially being better for HRV.
Consult a cardiologist or autonomic specialist to assess individual needs regarding beta blockers and HRV.